Blog
Read stories and case studies from our work at the intersection of strategy, design, and impact. From evaluation insights to community-driven campaigns, we break down how data and storytelling drive better public health outcomes.
Framing Public Health Systems Change:
A Micro, Meso, and Macro Level Overview
Public health systems are complex, adaptive, and constantly evolving. Change doesn’t happen in silos, and effective transformation requires us to understand how actors and actions across different levels of influence interact. At Impact Narrative Consulting, we use a systems-level framing adapted from Kirchherr et al. (2021) to help public health leaders think across three interconnected levels: micro, meso, and macro. Our framework translates these concepts to public health practice, aligning responsibility and strategy based on proximity to community, institutional power, and resource capacity.
Micro Level: Frontline Public Health Professionals
The micro level refers to individuals working directly with communities, Community Health Workers (CHWs), health educators, peer support specialists, and other frontline practitioners. These professionals are closest to the people and communities they serve. They provide essential services, help clients navigate complex systems, and hold valuable insight into local barriers, gaps, and cultural nuances.
Responsibilities at the micro level should match available capacity, ensuring these professionals aren’t weighed down with systemic accountability that exceeds their power or resources. Core functions often include:
- Delivering patient-centered care and health education tailored to community needs
- Participating in professional development, skill-building, and peer learning opportunities
- Collaborating with cross-sector teams (e.g., case managers, social workers) to coordinate services
- Providing feedback to organizations based on lived community experience
- Contributing to equitable and accessible data collection, including reviewing results and informing next steps
- Mentoring peers and supporting onboarding for new workforce members
- Building and maintaining networks to share resources, best practices, and emerging solutions
- Engaging in strategic partnerships that connect clients to community and human services
- Taking part in committees, workgroups, and leadership opportunities to represent frontline perspectives
- Practicing burnout prevention and peer support to sustain workforce wellbeing
This level also depends on strong support systems, such as peer mentorship, leadership development pathways, and comprehensive onboarding, that equip individuals to thrive without isolating them with responsibility for system-wide challenges.
Meso Level: Public Health Organizations and Institutions
The meso level includes the structures that employ and support public health professional, health departments, nonprofit agencies, clinics, hospitals, and community-based organizations. These entities design and implement programs, manage funding, oversee supervision, and directly influence how frontline roles are valued and supported.
Organizations must carry the structural responsibility for enabling effective service delivery. They are positioned to:
- Provide training, technology, and tools necessary to equip staff for high-quality service delivery
- Ensure transportation, facility access, and client communication resources are available
- Build standardized workflows and referral/resource systems that are streamlined, reliable, and reduce administrative burden
- Develop infrastructure that supports burnout prevention and sustainable workloads
- Institutionalize equity, reciprocity, and inclusion into hiring, evaluation, and leadership practices
- Offer tailored supervision and professional development based on role-specific needs
- Facilitate cross-department and cross-organization collaboration to close service gaps and improve continuity of care
- Create meaningful opportunities for frontline professionals to co-design programs, contribute to decision-making, and inform organizational strategy
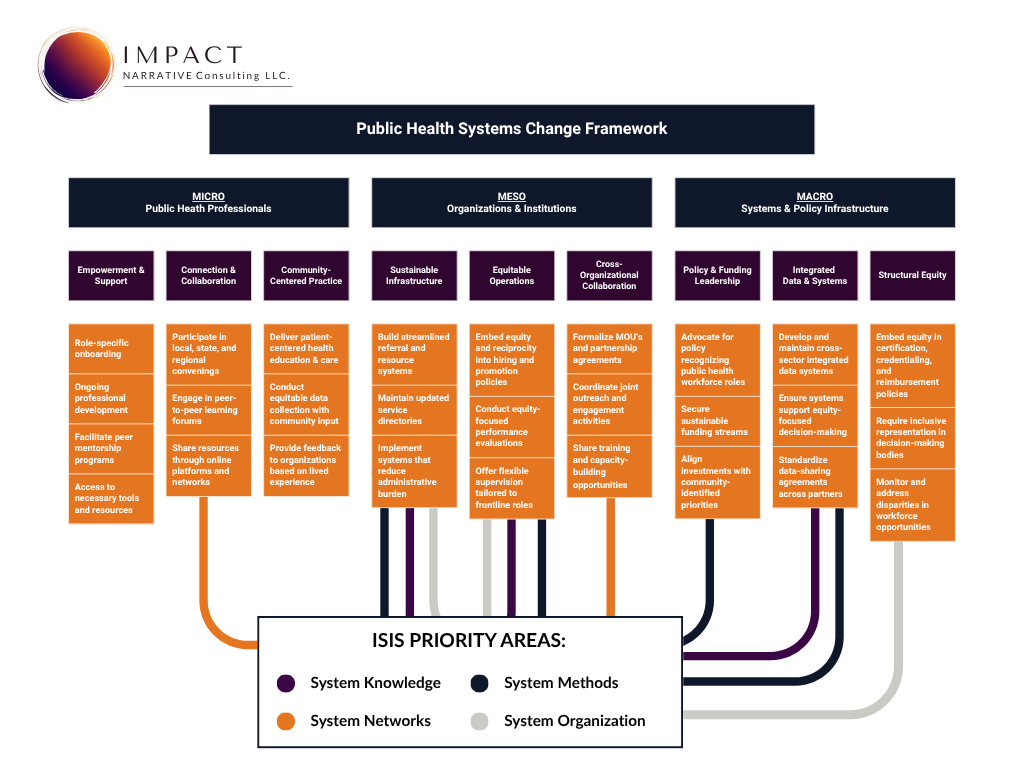
Many of these responsibilities align with the Initiative on the Study and Implementation of Systems (ISIS) framework. At the meso level, organizations operationalize macro-level infrastructure by adopting systems knowledge management tools, contributing to shared datasets, and applying participatory systems methods, such as concept mapping or service mapping, to co-design interventions with staff and community partners. They also strengthen system networks by building direct connections with other organizations, aligning referral pathways, and sharing resources to reduce duplication and close service gaps.
Meso-level actors bridge the gap between policy and practice. They are essential for translating macro-level strategies into the daily realities of public health service delivery.
Macro Level: Systems and Policy Infrastructure
At the macro level, we look at governmental systems, funders, policymakers, credentialing bodies, and multisector coalitions. This level has the most structural power and resource capacity, and should therefore bear the greatest responsibility for driving large-scale, sustainable change.
Macro-level action includes:
- Developing policy that formally recognizes and invests in the public health workforce
- Aligning funding streams with both community priorities and workforce capacity needs
- Creating and maintaining integrated data systems that inform equity-focused planning and interventions
- Embedding equity and reciprocity into certification, credentialing, and reimbursement structures
- Using data-driven insights to guide system-wide resource allocation and reform
The macro level carries the responsibility for enabling and sustaining the four ISIS priority areas at scale. This includes creating the policy, funding, and infrastructure to maintain collaborative knowledge management systems, build and connect multilevel networks, invest in systems modeling and evaluation, and promote adaptive governance structures that replace siloed, top-down approaches with participatory decision-making. Without these enabling conditions, meso-level organizations and micro-level professionals cannot fully realize their potential for impact.
These systemic levers establish the conditions for meso and micro levels to function equitably and effectively. They are the foundation for lasting transformation in public health.
Why It Matters: Aligning Power, Responsibility, and Impact
One of the most persistent barriers to public health systems change is misaligned responsibility, when the burden of addressing structural challenges falls on those with the least power, resources, or authority to act. Too often, frontline professionals at the micro level are expected to solve systemic problems without the infrastructure or policy support they need.
This framework offers a clearer path forward by matching responsibility with capacity:
- Micro level actors should be empowered through resources, training, and leadership opportunities, without being overburdened by structural accountability.
- Meso level institutions must own the responsibility for building sustainable infrastructure, reducing barriers, and creating the conditions for frontline roles to succeed.
- Macro level systems should lead on policy reform, funding alignment, and large-scale structural changes that enable equitable, effective public health delivery.
By aligning power with responsibility, we create a foundation for stronger accountability, better collaboration, and more targeted evaluation. This alignment also improves how programs are designed, how resources are distributed, and how success is measured.
Grounded in Systems Thinking
This framework is adapted from Kirchherr et al. (2021), who outlined macro–meso–micro system actors in the context of circular economies. We have translated their model into a public health context, with clear roles for frontline professionals, organizations, and system-level actors.
It is also informed by Leischow et al. (2008), whose work on systems thinking in tobacco control demonstrates the value of networked, collaborative, and adaptive strategies, and by the classic Levels of Prevention model from Leavell & Clark, which emphasizes the timing and scope of interventions.
Locally, this thinking aligns closely with the Cultivating Community Change Together comprehensive action plan developed through the Community Health Worker Initiative (CHWI) in Mecklenburg County. That plan outlines strategies at the CHW, organizational, and network levels, paralleling the micro, meso, and macro roles in our framework. By integrating CHWI’s locally driven strategies with a broader systems-thinking model, we can ensure that change efforts are both context-specific and structurally aligned across all levels of influence.
This approach also draws on the Initiative on the Study and Implementation of Systems (ISIS) framework, which identifies four priority areas for strengthening public health systems: systems knowledge management, systems networks, systems methods, and systems organization. These priorities require coordinated action across macro and meso levels, macro actors build and resource the infrastructure, while meso actors integrate and apply these capabilities within their organizational practice. Together, they create the conditions for micro-level professionals to focus on what they do best: delivering high-quality, community-informed public health services.
These approaches share a common principle: improving health outcomes requires understanding complexity, modeling relationships, and designing solutions with, not for, the people and organizations involved. Public health systems change is most successful when it is co-created, data-informed, and aligned across all levels of the system.
References
- Kirchherr, J., et al. (2021). The system-level approach to the circular economy: describing actors on the macro, meso, and micro levels. ResearchGate
- Leischow, S.J., et al. (2008). Systems thinking to improve the public’s health. American Journal of Preventive Medicine, 35(2 Suppl), S196–S203. PMC Article
- Leavell, H.R., & Clark, E.G. (1953). Preventive Medicine for the Doctor in His Community: An Epidemiologic Approach. McGraw-Hill.
- Mecklenburg County Public Health – Community Health Worker Initiative (CHWI). (2024). Cultivating Community Change Together: Mecklenburg County’s Community Health Worker Initiative Comprehensive Action Plan to Improve Access to Care. MeckNC Widen Library
Ready to Align Strategy With Impact?
Impact Narrative Consulting helps public health teams and organizations design outcome-driven evaluation plans grounded in systems thinking, equity, and Collective Impact.

